Fill Out a Valid Advance Beneficiary Notice of Non-coverage Template
Form Specs
| Fact Name | Description |
|---|---|
| Purpose | The Advance Beneficiary Notice of Non-coverage (ABN) informs Medicare beneficiaries that a service may not be covered by Medicare. |
| Required Use | Providers must issue an ABN when they believe that Medicare may deny payment for a service or item. |
| Beneficiary Rights | Beneficiaries can choose to accept or decline the service after receiving the ABN, understanding they may be responsible for payment. |
| State-Specific Laws | State laws may vary. For example, California requires compliance with state health care laws in addition to federal regulations. |
Dos and Don'ts
When filling out the Advance Beneficiary Notice of Non-coverage (ABN) form, it's essential to be mindful of certain dos and don'ts to ensure the process goes smoothly. Here’s a helpful guide:
- Do read the instructions carefully before starting to fill out the form.
- Do provide accurate and complete information to avoid delays.
- Do ensure that the patient understands the implications of signing the ABN.
- Do keep a copy of the signed ABN for your records.
- Don't rush through the form; take your time to ensure everything is correct.
- Don't leave any sections blank; incomplete forms can lead to confusion.
- Don't forget to explain the reason for non-coverage to the patient clearly.
Other PDF Documents
6 Team Consolation Bracket - Facilitates the tracking of game results systematically.
For those looking to navigate the process of vehicle ownership transfer, the Texas Motor Vehicle Bill of Sale form is indispensable. It not only documents the sale but also protects both parties by providing clear evidence of the transaction. To gain further insight into this essential legal document and to access a template, read here.
Employer's Quarterly Federal Tax Return - Filing Form 941 is necessary for claiming certain payroll tax credits and benefits.
Common mistakes
-
Not reading the instructions carefully. Many people skip over the instructions, leading to mistakes that could have been avoided. It’s essential to understand the purpose of the form before filling it out.
-
Failing to provide accurate personal information. It’s crucial to enter your name, Medicare number, and other identifying details correctly. Any errors can cause delays in processing.
-
Not checking the date. Forgetting to include the date when signing the form can lead to complications. Always ensure the date is current and legible.
-
Overlooking the service description. When listing the services or items in question, be specific. Vague descriptions can lead to confusion and potential denial of coverage.
-
Neglecting to sign the form. A signature is necessary for the form to be valid. Without it, the form may be considered incomplete.
-
Not understanding the implications of the notice. Some individuals do not fully grasp what it means to receive an Advance Beneficiary Notice of Non-coverage. It’s important to understand that this notice indicates that Medicare may not cover the service.
-
Ignoring deadlines. There are specific timeframes for submitting the form. Missing these deadlines can result in loss of coverage or benefits.
-
Submitting the form without making copies. Keeping a copy of the completed form for your records is vital. If any issues arise, having a copy can be very helpful.
-
Not asking for help. Many people feel embarrassed to ask questions or seek assistance. However, it’s perfectly acceptable to ask for clarification when needed.
-
Failing to follow up. After submitting the form, it’s important to follow up to ensure that it has been received and processed correctly. Checking in can prevent future issues.
Documents used along the form
The Advance Beneficiary Notice of Non-coverage (ABN) form is a critical document used in healthcare settings to inform patients about services that Medicare may not cover. Along with the ABN, several other forms and documents often accompany the process of managing patient care and billing. Below is a list of these documents, each serving a specific purpose in the healthcare system.
- Medicare Claim Form (CMS-1500): This form is used by healthcare providers to bill Medicare for services rendered to patients. It includes details about the patient, the services provided, and the costs involved.
- Patient Authorization Form: This document allows healthcare providers to share a patient’s medical information with other entities, such as insurance companies or specialists, ensuring compliance with privacy regulations.
- Notice of Privacy Practices: Patients receive this notice to understand how their medical information may be used and disclosed. It outlines their rights regarding their health information.
- Medicare Summary Notice (MSN): This is a statement sent to Medicare beneficiaries that outlines the services received, the amounts billed, and what Medicare paid. It helps patients understand their financial responsibilities.
- Power of Attorney form: It allows an individual to appoint an agent for decision-making on their behalf, covering financial matters and healthcare choices. Understanding this document ensures that one's wishes are respected. For more details, visit Forms Washington.
- Authorization for Release of Medical Records: This form permits healthcare providers to release a patient's medical records to a specified individual or entity, facilitating continuity of care.
- Financial Responsibility Agreement: Patients may sign this document to acknowledge their understanding of the financial obligations associated with their care, including co-pays and deductibles.
- Referral Form: A referral form is used when a primary care physician directs a patient to a specialist for further evaluation or treatment, ensuring proper communication between providers.
- Patient Satisfaction Survey: This survey gathers feedback from patients about their healthcare experience, allowing providers to improve service quality and patient care.
- Durable Medical Equipment (DME) Prescription: This document is necessary for patients who require medical equipment, such as wheelchairs or oxygen tanks, and must be completed by a healthcare provider.
These forms and documents play essential roles in the healthcare process, ensuring that patients are informed, their rights are protected, and that billing and care coordination are handled efficiently. Understanding these documents can help patients navigate their healthcare experience more effectively.
Misconceptions
- Misconception 1: The ABN is only for Medicare patients.
- Misconception 2: Signing an ABN means you are agreeing to pay for the service.
- Misconception 3: The ABN guarantees that the service will be covered.
- Misconception 4: You cannot appeal a decision if you receive an ABN.
- Misconception 5: All providers are required to issue an ABN.
- Misconception 6: An ABN is the same as a waiver of liability.
- Misconception 7: You must always pay for services if you receive an ABN.
- Misconception 8: An ABN is only necessary for expensive procedures.
This is not true. While the ABN is primarily associated with Medicare, it can also be relevant for other insurance plans that require prior authorization or have specific coverage criteria.
Signing the ABN indicates that you understand the service may not be covered. It does not automatically mean you are responsible for payment; coverage determination will still be made by your insurer.
The ABN does not guarantee coverage. It simply informs you that the provider believes the service may not be covered, and it outlines your options.
You still have the right to appeal if a service is denied after receiving an ABN. The form does not waive your right to contest the coverage decision.
Not all providers are required to issue an ABN. It is only necessary when a provider believes that a service may not be covered by Medicare or other insurance.
The ABN and a waiver of liability serve different purposes. The ABN informs you about potential non-coverage, while a waiver of liability protects the provider from financial responsibility if a service is denied.
Receiving an ABN does not mean you must pay for the service upfront. It simply means that coverage is uncertain, and you should discuss payment options with your provider.
ABNs can be issued for any service that may not be covered, regardless of cost. It is important to be informed about coverage for all types of services.
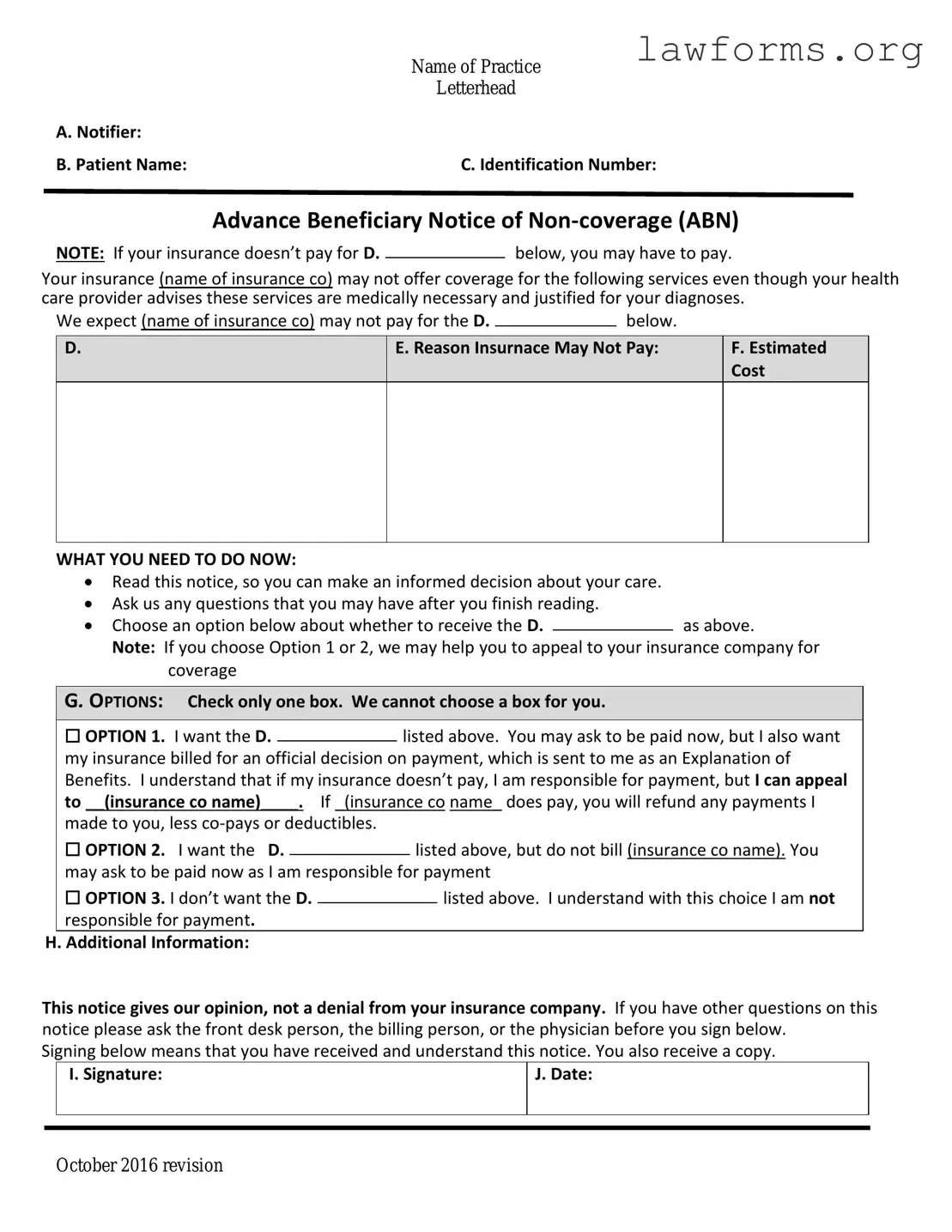
Preview - Advance Beneficiary Notice of Non-coverage Form
|
Name of Practice |
|
Letterhead |
A. Notifier: |
|
B. Patient Name: |
C. Identification Number: |
Advance Beneficiary Notice of
NOTE: If your insurance doesn’t pay for D.below, you may have to pay.
Your insurance (name of insurance co) may not offer coverage for the following services even though your health care provider advises these services are medically necessary and justified for your diagnoses.
We expect (name of insurance co) may not pay for the D. |
|
below. |
|
D.
E. Reason Insurnace May Not Pay:
F.Estimated Cost
WHAT YOU NEED TO DO NOW:
Read this notice, so you can make an informed decision about your care.
Ask us any questions that you may have after you finish reading.
Choose an option below about whether to receive the D.as above.
Note: If you choose Option 1 or 2, we may help you to appeal to your insurance company for coverage
G. OPTIONS: Check only one box. We cannot choose a box for you.
|
☐ OPTION 1. I want the D. |
|
listed above. You may ask to be paid now, but I also want |
||||
|
|
||||||
|
my insurance billed for an official decision on payment, which is sent to me as an Explanation of |
||||||
|
Benefits. I understand that if my insurance doesn’t pay, I am responsible for payment, but I can appeal |
||||||
|
to __(insurance co name)____. If _(insurance co name_ does pay, you will refund any payments I |
||||||
|
made to you, less |
|
|
|
|||
|
☐ OPTION 2. I want the D. |
|
|
listed above, but do not bill (insurance co name). You |
|||
|
|
|
|||||
|
may ask to be paid now as I am responsible for payment |
||||||
|
☐ OPTION 3. I don’t want the D. |
|
|
|
listed above. I understand with this choice I am not |
||
|
|
|
|
||||
|
responsible for payment. |
|
|
|
|||
H. Additional Information: |
|
|
|
||||
This notice gives our opinion, not a denial from your insurance company. If you have other questions on this notice please ask the front desk person, the billing person, or the physician before you sign below.
Signing below means that you have received and understand this notice. You also receive a copy.
|
I. Signature: |
J. Date: |
|
|
|
|
|
|
October 2016 revision
Key takeaways
The Advance Beneficiary Notice of Non-coverage (ABN) form is an important document for Medicare beneficiaries. Understanding how to fill it out and use it effectively can help avoid unexpected medical costs. Here are key takeaways regarding the ABN form:
- The ABN is used to inform beneficiaries that Medicare may not cover a specific service or item.
- It must be filled out before the service is provided, ensuring that the beneficiary is aware of potential out-of-pocket expenses.
- Beneficiaries should read the notice carefully, as it outlines the reasons for non-coverage.
- Signing the ABN indicates that the beneficiary accepts financial responsibility if Medicare denies payment.
- Providers must retain a copy of the signed ABN in the beneficiary's medical record.
- Beneficiaries can appeal Medicare's decision if they believe the service should be covered.
Using the ABN correctly can help beneficiaries make informed decisions about their healthcare services.
Similar forms
- Medicare Summary Notice (MSN): This document provides a summary of the services provided to a beneficiary and details any payments made by Medicare. It informs beneficiaries about what was covered and what they may be responsible for paying.
- Homeschool Letter of Intent: This form is essential for parents planning to homeschool, as it formally expresses their intent to the state. Completing this form accurately is crucial for adherence to legal requirements while homeschooling. For more information, visit https://californiadocsonline.com/homeschool-letter-of-intent-form.
- Explanation of Benefits (EOB): Issued by private insurers, this document outlines the services received, the amount billed, and how much the insurance will pay. It also indicates any remaining balance that the beneficiary must cover.
- Notice of Privacy Practices: This document informs patients about how their health information may be used and shared. It is similar in that it ensures transparency and informs individuals about their rights regarding their health information.
- Prior Authorization Request: This is a form that healthcare providers submit to insurance companies to obtain approval for certain services before they are provided. It serves to inform patients about whether a service is likely to be covered, similar to the Advance Beneficiary Notice.
- Patient Responsibility Statement: This document outlines the patient's financial responsibility for services rendered. It is akin to the Advance Beneficiary Notice in that it clarifies potential costs that the patient may incur.
- Claim Denial Letter: When a claim for coverage is denied, this letter explains the reasons for the denial. Like the Advance Beneficiary Notice, it communicates important information about coverage decisions.
- Out-of-Pocket Cost Estimate: This estimate provides patients with an idea of their potential out-of-pocket expenses for upcoming services. It is similar in that it helps beneficiaries understand their financial obligations ahead of time.
- Medicare Enrollment Confirmation: This document confirms a beneficiary's enrollment in Medicare and outlines the benefits available. It serves as a foundational communication, much like the Advance Beneficiary Notice, which informs beneficiaries about their coverage options.