Attorney-Approved Do Not Resuscitate Order Template for the State of Florida
Form Specifications
| Fact Name | Description |
|---|---|
| Definition | The Florida Do Not Resuscitate (DNR) Order is a legal document that allows individuals to refuse resuscitation efforts in the event of a cardiac or respiratory arrest. |
| Governing Law | The Florida DNR Order is governed by Florida Statutes, specifically Section 401.45. |
| Eligibility | Any adult can complete a DNR order, but it must be signed by a licensed physician to be valid. |
| Form Availability | The Florida DNR Order form is available online through the Florida Department of Health website and can be printed for use. |
| Signature Requirement | The DNR order must be signed by the patient or their legal representative, along with the physician's signature. |
| Healthcare Provider Obligations | Healthcare providers are required to honor a valid DNR order and cannot perform resuscitation efforts if one is present. |
| Revocation | A DNR order can be revoked at any time by the patient or their legal representative, verbally or in writing. |
| Emergency Medical Services | Emergency Medical Services (EMS) personnel must be able to clearly identify a DNR order to respect the patient's wishes. |
| Storage and Accessibility | It is recommended that individuals keep their DNR order in an easily accessible location, such as on the refrigerator or with their medical records. |
| Limitations | A DNR order only applies to resuscitation efforts and does not affect other medical treatments or care decisions. |
Dos and Don'ts
When filling out the Florida Do Not Resuscitate Order form, it's important to follow certain guidelines to ensure your wishes are clearly understood. Here’s a list of things you should and shouldn't do:
- Do discuss your wishes with your family and healthcare provider.
- Do ensure the form is signed and dated by you or your legal representative.
- Do keep a copy of the completed form in an accessible location.
- Do review the form regularly to make sure it still reflects your wishes.
- Don't leave the form unsigned or undated.
- Don't assume that verbal instructions are enough; written documentation is necessary.
- Don't forget to inform your healthcare providers about the existence of the form.
- Don't ignore state-specific requirements when filling out the form.
Create Popular Do Not Resuscitate Order Forms for Different States
Can a Family Member Override a Dnr - A DNR order can change based on the patient's health status or personal beliefs.
How Old Do You Have to Be to Sign a Dnr - This order prioritizes the dignity and comfort of the patient.
Dnr Rules and Regulations - The DNR form should be understood completely before signing to ensure that all parties are informed.
A California Hold Harmless Agreement is a legal document designed to protect one party from liability for certain actions or events. This form is commonly used in various situations, such as contracts and rental agreements, where one party agrees to assume the risk and hold another party harmless from any potential claims. For detailed information and to access the agreement, visit californiadocsonline.com/hold-harmless-agreement-form/. Understanding this agreement is essential for anyone looking to navigate liability issues effectively in California.
What Is a Dnr - A Do Not Resuscitate Order is a legal document indicating a patient's wishes regarding resuscitation efforts.
Common mistakes
-
Not understanding the purpose of the form: Many individuals fill out the Do Not Resuscitate Order (DNRO) without fully grasping its implications. This can lead to decisions that may not align with their wishes regarding end-of-life care.
-
Failing to discuss with family: Some people do not talk about their decision with family members. This can cause confusion and emotional distress for loved ones during critical moments.
-
Incorrectly filling out personal information: Errors in providing name, date of birth, or other identifying details can render the form invalid. It is essential to double-check all information.
-
Not signing the form: A common oversight is forgetting to sign the DNRO. Without a signature, the document may not be legally recognized.
-
Neglecting witness requirements: In Florida, the DNRO must be signed in the presence of two witnesses or a notary. Failing to meet this requirement can invalidate the order.
-
Using outdated forms: Some individuals may use old versions of the DNRO. It is important to ensure that the most current form is being utilized to avoid issues.
-
Not reviewing the form regularly: Life circumstances can change. Failing to review and update the DNRO can lead to a situation where the document no longer reflects one’s current wishes.
-
Overlooking the need for copies: After completing the DNRO, individuals often forget to make copies for their medical providers and family members. Having multiple copies ensures that the order is accessible when needed.
-
Ignoring state-specific regulations: Each state has its own rules regarding DNROs. Not adhering to Florida’s specific requirements can lead to complications or misunderstandings in medical settings.
-
Assuming verbal instructions are sufficient: Some people believe that simply telling healthcare providers their wishes is enough. However, without a written and signed DNRO, those wishes may not be honored.
Documents used along the form
When considering end-of-life care options in Florida, the Do Not Resuscitate (DNR) Order is a critical document. However, it is often accompanied by other important forms that help clarify a person’s wishes regarding medical treatment. Understanding these documents can empower individuals and their families to make informed decisions about healthcare preferences.
- Advance Directive: This document outlines a person's wishes regarding medical treatment and can include preferences for life-sustaining measures. It provides guidance to healthcare providers and loved ones if the individual becomes unable to communicate their desires.
- Healthcare Surrogate Designation: This form allows an individual to appoint someone to make healthcare decisions on their behalf if they are unable to do so. This trusted person can ensure that the individual's wishes are respected and followed.
- Living Will: A living will specifies the types of medical treatment a person does or does not want in the event of a terminal illness or irreversible condition. It is a vital tool for communicating one's preferences regarding end-of-life care.
- Physician Orders for Life-Sustaining Treatment (POLST): This document translates a patient's wishes into actionable medical orders. It is particularly useful for individuals with serious illnesses and ensures that their treatment preferences are honored by healthcare providers.
- Do Not Hospitalize (DNH) Order: This order indicates that a patient should not be transferred to a hospital for treatment. It is often used for patients in long-term care facilities who wish to avoid hospitalization in certain situations.
- Organ Donation Registration: This form allows individuals to express their wishes regarding organ donation. It ensures that healthcare providers are aware of the individual's intent to donate organs after death.
- Operating Agreement: This document is essential for LLCs as it defines the operational procedures and organizational structure, ensuring clarity among members, similar to how other legal documents like the formsillinois.com aid in healthcare decisions.
- Medical Power of Attorney: This legal document grants someone the authority to make healthcare decisions on behalf of another person. It is essential for ensuring that someone trusted can advocate for the individual's medical preferences.
- Patient Advocate Designation: Similar to a healthcare surrogate, this document allows an individual to appoint someone to advocate for their rights and preferences in healthcare settings, ensuring their voice is heard even when they cannot speak for themselves.
Understanding these documents can greatly enhance the ability to navigate complex healthcare decisions. Each form serves a unique purpose and collectively helps ensure that an individual's healthcare preferences are respected and upheld. Taking the time to complete these documents can provide peace of mind for both the individual and their loved ones.
Misconceptions
Many people hold misconceptions about the Florida Do Not Resuscitate Order (DNRO) form. Understanding these misconceptions is crucial for making informed decisions regarding end-of-life care. Here are six common misunderstandings:
- Misconception 1: A DNRO means that medical care will be completely withheld.
- Misconception 2: A DNRO is only for terminally ill patients.
- Misconception 3: A DNRO is a legally binding document that cannot be revoked.
- Misconception 4: A DNRO must be signed by a lawyer to be valid.
- Misconception 5: A DNRO is the same as a living will.
- Misconception 6: A DNRO is only valid in Florida.
This is incorrect. A DNRO specifically addresses resuscitation efforts in the event of cardiac arrest. Other medical treatments and interventions will still be provided as needed.
While many people associate DNROs with terminal illness, anyone can choose to have one, regardless of their current health status. It is a personal decision based on individual values and preferences.
This is false. Individuals can revoke a DNRO at any time. It is important to communicate any changes to healthcare providers and ensure that the new wishes are documented.
This is not true. In Florida, a DNRO must be completed and signed by a physician, but it does not require a lawyer's signature or involvement.
While both documents relate to end-of-life decisions, they serve different purposes. A living will outlines a person's wishes regarding medical treatment in situations where they cannot communicate, while a DNRO specifically addresses resuscitation efforts.
This is misleading. While the Florida DNRO is specific to the state, similar forms exist in other states. However, the legal requirements and implications may vary, so it is essential to understand the laws in each state.
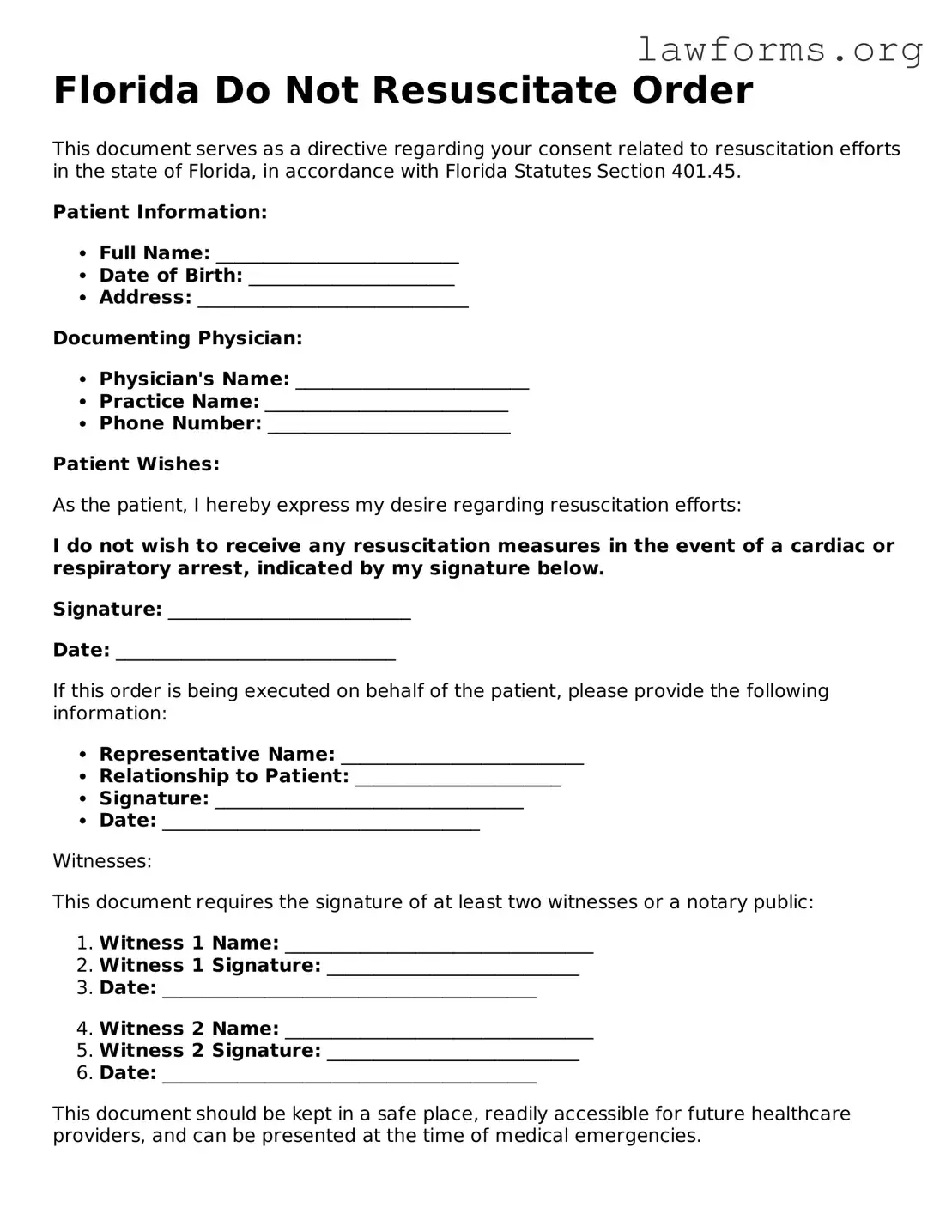
Preview - Florida Do Not Resuscitate Order Form
Florida Do Not Resuscitate Order
This document serves as a directive regarding your consent related to resuscitation efforts in the state of Florida, in accordance with Florida Statutes Section 401.45.
Patient Information:
- Full Name: __________________________
- Date of Birth: ______________________
- Address: _____________________________
Documenting Physician:
- Physician's Name: _________________________
- Practice Name: __________________________
- Phone Number: __________________________
Patient Wishes:
As the patient, I hereby express my desire regarding resuscitation efforts:
I do not wish to receive any resuscitation measures in the event of a cardiac or respiratory arrest, indicated by my signature below.
Signature: __________________________
Date: ______________________________
If this order is being executed on behalf of the patient, please provide the following information:
- Representative Name: __________________________
- Relationship to Patient: ______________________
- Signature: _________________________________
- Date: __________________________________
Witnesses:
This document requires the signature of at least two witnesses or a notary public:
- Witness 1 Name: _________________________________
- Witness 1 Signature: ___________________________
- Date: ________________________________________
- Witness 2 Name: _________________________________
- Witness 2 Signature: ___________________________
- Date: ________________________________________
This document should be kept in a safe place, readily accessible for future healthcare providers, and can be presented at the time of medical emergencies.
Key takeaways
Filling out a Do Not Resuscitate (DNR) Order in Florida can be an important step in ensuring that your healthcare preferences are respected. Here are some key takeaways to consider:
- Understand the Purpose: A DNR order indicates that you do not wish to receive cardiopulmonary resuscitation (CPR) in the event of cardiac arrest.
- Eligibility: Any adult can complete a DNR order, but it is often used by individuals with serious health conditions or those who are nearing the end of life.
- Consult with Healthcare Providers: Discuss your wishes with your doctor or healthcare provider to ensure that a DNR order aligns with your overall treatment plan.
- Complete the Form: The Florida DNR form must be filled out and signed by you and your physician. Make sure all required sections are completed.
- Keep Copies Accessible: After filling out the form, keep copies in easily accessible locations, such as with your medical records or at home.
- Inform Family Members: Share your decision and the location of the DNR order with family members and caregivers to avoid confusion during emergencies.
- Review and Update: Regularly review your DNR order, especially if your health status changes or if you wish to alter your preferences.
- Know Your Rights: You have the right to change or revoke your DNR order at any time. Be sure to communicate any changes to your healthcare team.
By understanding these key aspects, you can make informed decisions regarding your healthcare preferences and ensure that your wishes are honored.
Similar forms
- Living Will: This document outlines a person's wishes regarding medical treatment in situations where they cannot communicate their preferences. It often includes decisions about life-sustaining treatments.
- Healthcare Power of Attorney: This form designates an individual to make medical decisions on behalf of another person if they are unable to do so. It provides authority to act in accordance with the patient’s wishes.
- Advance Directive: An advance directive combines a living will and healthcare power of attorney. It provides clear instructions about medical care preferences and appoints someone to make decisions.
- Physician Orders for Life-Sustaining Treatment (POLST): This document translates a patient's wishes into medical orders. It is intended for patients with serious illnesses and ensures their preferences are honored across different care settings.
- Do Not Intubate (DNI) Order: Similar to a DNR, a DNI order specifically states that a patient should not be intubated if they experience respiratory failure. It focuses on breathing support decisions.
- Comfort Care Order: This order emphasizes providing comfort rather than curative treatment. It ensures that patients receive palliative care to manage pain and other distressing symptoms.
- Medical Orders for Scope of Treatment (MOST): This document is similar to POLST and is used to communicate a patient’s preferences for treatment options. It is often used in specific regions and healthcare systems.
- Emergency Medical Services (EMS) Do Not Resuscitate (DNR) Form: This form is specifically designed for emergency medical personnel. It communicates a patient's wishes regarding resuscitation in emergency situations.
Non-disclosure Agreement (NDA): This legal document is crucial for protecting sensitive information shared between parties. A well-drafted NDA ensures confidentiality and prevents unauthorized disclosure of proprietary details. For guidance on creating an NDA, you can refer to Forms Washington.
- Patient Autonomy Document: This document outlines a patient’s rights to make decisions about their own healthcare. It emphasizes the importance of respecting individual choices regarding treatment.