Attorney-Approved Do Not Resuscitate Order Template for the State of New Jersey
Form Specifications
| Fact Name | Details |
|---|---|
| Definition | A Do Not Resuscitate (DNR) Order in New Jersey is a legal document that instructs medical personnel not to perform cardiopulmonary resuscitation (CPR) in the event of cardiac arrest. |
| Governing Law | The New Jersey Do Not Resuscitate Order is governed by the New Jersey Advance Directives for Health Care Act, N.J.S.A. 26:2H-53 et seq. |
| Eligibility | Any adult who is capable of making their own medical decisions can complete a DNR Order. This includes individuals with terminal illnesses or those who wish to refuse resuscitation. |
| Form Requirements | The DNR Order must be signed by the patient or their authorized representative and a physician. It must also be in writing to be valid. |
| Implementation | Once completed, the DNR Order should be prominently displayed in the patient’s medical records and made available to emergency medical personnel. |
| Revocation | A DNR Order can be revoked at any time by the patient or their representative, verbally or in writing, as long as the revocation is communicated clearly. |
Dos and Don'ts
When filling out the New Jersey Do Not Resuscitate Order form, it is important to follow certain guidelines to ensure clarity and compliance. Here are five things to do and five things to avoid:
- Do ensure that the form is signed by a physician. This signature is crucial for the order to be valid.
- Do provide accurate personal information, including your full name, date of birth, and any relevant medical history.
- Do discuss your wishes with family members and healthcare providers. Open communication can prevent confusion later.
- Do keep a copy of the completed form in an accessible location. This ensures that it can be easily found in an emergency.
- Do review the form periodically. Changes in your health or preferences may require updates to the order.
- Don't leave any sections of the form blank. Incomplete information can lead to misunderstandings.
- Don't assume that verbal instructions are sufficient. Written documentation is necessary for legal purposes.
- Don't forget to inform your healthcare provider that you have completed the form. They need to be aware of your wishes.
- Don't use outdated versions of the form. Always check for the most current version to ensure compliance.
- Don't overlook the importance of discussing your decision with a legal advisor if you have concerns about the implications.
Create Popular Do Not Resuscitate Order Forms for Different States
Dnr Rules and Regulations - Creating a DNR order requires informed consent from the patient or their legally authorized representative.
It is essential for both buyers and sellers to understand the significance of the Texas Motor Vehicle Bill of Sale form in documenting the sale of a vehicle. This vital document not only records the transaction but also protects the interests of both parties involved. For more detailed information on filling out this form accurately, you can read here.
Printable Dnr Form - Regular review of the order is recommended to ensure it reflects current wishes as circumstances change.
Common mistakes
-
Failing to clearly identify the patient. It is essential to provide accurate personal information, including the full name and date of birth.
-
Not signing the form. A signature is required to validate the order. Without it, the document holds no legal weight.
-
Using outdated forms. Always ensure that you have the most recent version of the Do Not Resuscitate Order form to avoid legal complications.
-
Inadequately discussing the order with healthcare providers. Conversations with medical professionals help clarify the implications of the order.
-
Not involving family members. It is crucial to discuss the decision with loved ones, as they may need to advocate for the patient’s wishes.
-
Leaving sections of the form blank. Each part of the form serves a purpose. Omitting information can lead to misunderstandings.
-
Misunderstanding the medical terminology. If any terms are unclear, seek clarification to ensure the order reflects the patient’s wishes.
-
Failing to update the order. Life circumstances change. Regularly review and revise the order as needed.
-
Not keeping copies of the signed form. It is important to retain copies for personal records and to share with healthcare providers.
Documents used along the form
The New Jersey Do Not Resuscitate (DNR) Order form is an important document for individuals who wish to express their preferences regarding resuscitation efforts in the event of a medical emergency. Several other forms and documents may accompany the DNR Order to ensure comprehensive end-of-life planning and decision-making. Below is a list of commonly used documents that may be relevant.
- Advance Directive: This document outlines an individual's preferences for medical treatment in situations where they cannot communicate their wishes. It can include decisions about life-sustaining treatment and appointing a healthcare proxy.
- Living Will: A living will specifies an individual's wishes regarding medical treatment, particularly in scenarios involving terminal illness or irreversible conditions. It serves as a guide for healthcare providers and family members.
- Healthcare Proxy: This document designates a person to make healthcare decisions on behalf of an individual if they become unable to do so. It is crucial for ensuring that a person's medical preferences are honored.
- Physician Orders for Life-Sustaining Treatment (POLST): POLST is a medical order that specifies the types of medical treatment a patient wishes to receive during a medical emergency. It is designed for individuals with serious health conditions.
- Notary Acknowledgement Form: To secure your transactions, refer to our essential Notary Acknowledgement guidelines for accurate verification of signatures.
- Patient Identification Wristband: A wristband indicating a DNR status can be used in medical settings to quickly communicate a patient's wishes to healthcare providers during emergencies.
- Do Not Hospitalize (DNH) Order: This order is used to prevent hospitalization for individuals who prefer to receive care in a home or hospice setting, emphasizing comfort over aggressive treatment.
- Emergency Medical Services (EMS) DNR Form: This form is specifically designed for use by emergency medical services personnel. It ensures that the DNR order is recognized and followed in pre-hospital settings.
Each of these documents plays a vital role in ensuring that an individual's healthcare preferences are respected and followed. It is essential to consider these forms when planning for end-of-life care and to discuss them with family members and healthcare providers.
Misconceptions
Understanding the New Jersey Do Not Resuscitate (DNR) Order form is crucial for individuals and families making end-of-life decisions. However, several misconceptions can create confusion. Here are six common misunderstandings:
-
A DNR means no medical care at all.
This is not true. A DNR specifically addresses resuscitation efforts, such as CPR, in the event of cardiac arrest. It does not prevent you from receiving other forms of medical treatment or care.
-
Only terminally ill patients can have a DNR.
This misconception overlooks the fact that any individual, regardless of their health status, can request a DNR order. It is a personal choice based on individual values and preferences.
-
A DNR is a legally binding document that cannot be changed.
While a DNR is a legal document, it can be revoked or modified at any time by the individual or their authorized representative. It is important to communicate any changes to healthcare providers.
-
Having a DNR means you are giving up on life.
This belief can be disheartening. A DNR reflects a choice about how one wishes to approach end-of-life care, emphasizing comfort and quality of life rather than aggressive interventions.
-
All healthcare providers understand my DNR wishes.
While many providers are familiar with DNR orders, it is essential to ensure that your wishes are clearly communicated and documented. Discuss your DNR status with your healthcare team and family members.
-
A DNR is only for use in hospitals.
This is a common misunderstanding. A DNR can be applicable in various settings, including at home or in nursing facilities. It is important to ensure that your wishes are respected wherever you receive care.
By clarifying these misconceptions, individuals can make informed decisions about their healthcare preferences and ensure that their choices are respected in critical situations.
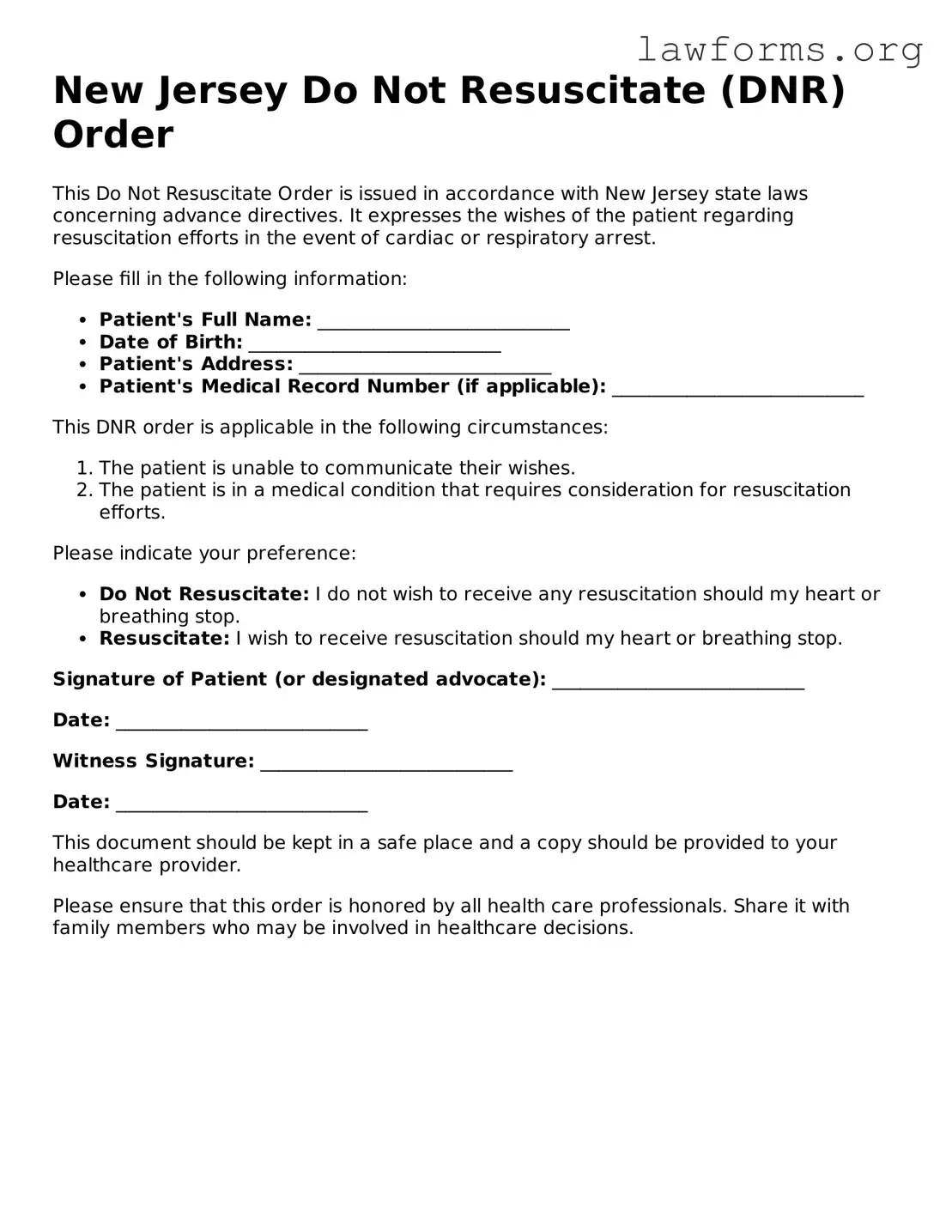
Preview - New Jersey Do Not Resuscitate Order Form
New Jersey Do Not Resuscitate (DNR) Order
This Do Not Resuscitate Order is issued in accordance with New Jersey state laws concerning advance directives. It expresses the wishes of the patient regarding resuscitation efforts in the event of cardiac or respiratory arrest.
Please fill in the following information:
- Patient's Full Name: ___________________________
- Date of Birth: ___________________________
- Patient's Address: ___________________________
- Patient's Medical Record Number (if applicable): ___________________________
This DNR order is applicable in the following circumstances:
- The patient is unable to communicate their wishes.
- The patient is in a medical condition that requires consideration for resuscitation efforts.
Please indicate your preference:
- Do Not Resuscitate: I do not wish to receive any resuscitation should my heart or breathing stop.
- Resuscitate: I wish to receive resuscitation should my heart or breathing stop.
Signature of Patient (or designated advocate): ___________________________
Date: ___________________________
Witness Signature: ___________________________
Date: ___________________________
This document should be kept in a safe place and a copy should be provided to your healthcare provider.
Please ensure that this order is honored by all health care professionals. Share it with family members who may be involved in healthcare decisions.
Key takeaways
When considering the New Jersey Do Not Resuscitate Order (DNR) form, it’s important to understand its purpose and how to properly use it. Here are some key takeaways:
- The DNR form allows individuals to express their wishes regarding resuscitation in case of a medical emergency.
- It must be completed and signed by a physician, ensuring that your wishes are legally recognized.
- Keep the DNR form in a visible place, such as on your refrigerator or with your medical records, so that emergency personnel can easily find it.
- Communicate your wishes with family members and healthcare providers to ensure everyone understands your decisions.
Similar forms
- Living Will: This document outlines a person's wishes regarding medical treatment in situations where they are unable to communicate. Like a DNR, it provides guidance to healthcare providers about the individual's preferences for end-of-life care.
- Healthcare Proxy: A healthcare proxy designates an individual to make medical decisions on behalf of someone else. This is similar to a DNR in that it ensures that a person's healthcare wishes are honored, particularly in critical situations.
- Advance Directive: An advance directive is a broader term that encompasses both living wills and healthcare proxies. It serves to communicate a person's healthcare preferences and can include instructions similar to those found in a DNR.
Non-disclosure Agreement (NDA): This essential legal document helps protect sensitive information shared between parties, ensuring that confidential details remain private. It is crucial for businesses and individuals looking to safeguard proprietary information. For a template, you can refer to Forms Washington.
- POLST (Physician Orders for Life-Sustaining Treatment): A POLST form is a medical order that details a patient's preferences for emergency medical treatment. It is similar to a DNR in that it provides specific instructions for healthcare providers in emergency situations.
- Medical Power of Attorney: This document grants someone the authority to make healthcare decisions on another person's behalf. It aligns with the purpose of a DNR by ensuring that medical choices reflect the patient's wishes, especially when they cannot express them.