Attorney-Approved Do Not Resuscitate Order Template for the State of Ohio
Form Specifications
| Fact Name | Details |
|---|---|
| Definition | The Ohio Do Not Resuscitate (DNR) Order form allows individuals to refuse resuscitation efforts in the event of a cardiac or respiratory arrest. |
| Governing Law | The DNR Order in Ohio is governed by Ohio Revised Code § 2133.21 to § 2133.26. |
| Eligibility | Any adult can complete a DNR Order, but it must be signed by a physician and the patient or their legal representative. |
| Form Availability | The DNR Order form is available through the Ohio Department of Health and various healthcare providers. |
| Emergency Medical Services | Emergency medical personnel are required to honor a valid DNR Order in accordance with Ohio law. |
| Revocation | A DNR Order can be revoked at any time by the patient or their legal representative, verbally or in writing. |
| Notification | It is recommended that individuals keep the DNR Order visible and notify family members and healthcare providers about its existence. |
Dos and Don'ts
When filling out the Ohio Do Not Resuscitate Order form, it is important to follow specific guidelines to ensure that the document is completed correctly. Below is a list of things you should and shouldn't do.
- Do ensure that the form is signed by a licensed physician.
- Do clearly indicate your wishes regarding resuscitation on the form.
- Do keep a copy of the completed form in an easily accessible location.
- Do discuss your decision with family members and healthcare providers.
- Don't leave any sections of the form blank.
- Don't forget to date the form when it is signed.
Create Popular Do Not Resuscitate Order Forms for Different States
Dnr Document - The order applies to cardiopulmonary resuscitation (CPR), which includes chest compressions and artificial ventilation.
In navigating the complexities of divorce, it is essential to have a comprehensive understanding of the documentation involved, particularly the Divorce Agreement, which serves as a crucial framework for both parties. This form not only delineates how assets and debts will be split but also addresses child custody and spousal support, facilitating a smoother transition into the next chapter of their lives.
Printable Dnr Form - Clear guidelines surrounding DNR orders can differ significantly between states; consult local resources.
Common mistakes
-
Not Understanding the Purpose: Many individuals fill out the Ohio Do Not Resuscitate Order form without fully grasping its intent. This document is not merely a refusal of treatment; it expresses a desire to avoid resuscitation in specific medical scenarios. Understanding this distinction is crucial.
-
Incomplete Information: A common error is failing to provide all necessary information on the form. Omitting details such as the patient’s full name, date of birth, or signature can render the document invalid. Each piece of information is vital to ensure the form is legally binding.
-
Inappropriate Signatures: The form requires signatures from the patient and, in some cases, a witness or healthcare provider. People often neglect to have the appropriate individuals sign the document. Without these signatures, the order may not be honored in a medical setting.
-
Failing to Discuss Wishes: It is essential to communicate your wishes with family members and healthcare providers before completing the form. Many people make the mistake of filling out the document without discussing their decisions with loved ones, leading to confusion or conflict during critical moments.
-
Not Updating the Form: Life circumstances change, and so may a person’s healthcare preferences. Individuals often overlook the need to review and update their Do Not Resuscitate Order. Regularly revisiting this document ensures that it reflects current wishes and medical conditions.
Documents used along the form
The Ohio Do Not Resuscitate (DNR) Order form is an essential document for individuals who wish to express their preferences regarding resuscitation efforts in medical emergencies. Alongside this form, several other documents can help clarify a person's healthcare wishes. Below is a list of commonly used forms that complement the DNR Order.
- Living Will: This document outlines a person's preferences for medical treatment in situations where they cannot communicate their wishes. It typically addresses end-of-life care and may include decisions about life-sustaining treatments.
- North Carolina Motor Vehicle Bill of Sale: This document serves as proof of purchase for a vehicle in North Carolina. To ensure the transfer of ownership is recorded accurately, it is important to properly complete the form. You can learn more about the document.
- Durable Power of Attorney for Healthcare: This form designates a specific person to make healthcare decisions on behalf of an individual if they become unable to do so themselves. It provides the appointed person with the authority to act according to the individual's wishes.
- Physician Orders for Life-Sustaining Treatment (POLST): POLST is a medical order that translates a patient’s wishes regarding treatment into actionable orders for healthcare providers. It is often used for individuals with serious illnesses or those nearing the end of life.
- Advance Directive: This broader term encompasses both living wills and durable powers of attorney. It allows individuals to communicate their healthcare preferences in advance, ensuring their wishes are respected.
- Healthcare Proxy: Similar to a durable power of attorney, this document appoints someone to make medical decisions on behalf of an individual. It is particularly useful when the individual cannot express their wishes due to incapacity.
- Do Not Intubate (DNI) Order: This order specifically instructs healthcare providers not to use intubation to assist with breathing. It is often used in conjunction with a DNR order to clarify treatment preferences further.
- Emergency Medical Services (EMS) Form: This form provides emergency responders with critical information about a patient’s wishes regarding resuscitation and other life-sustaining measures, ensuring that their preferences are honored in urgent situations.
Having these documents in place can provide clarity and peace of mind for both individuals and their loved ones. It ensures that healthcare providers understand and respect the wishes of patients during critical moments. By preparing these forms, individuals can take an active role in their healthcare decisions.
Misconceptions
Understanding the Ohio Do Not Resuscitate (DNR) Order form is crucial for individuals and families making end-of-life decisions. However, there are several misconceptions that can lead to confusion. Here are eight common misunderstandings:
- A DNR means no medical treatment at all. This is not true. A DNR specifically relates to resuscitation efforts in the event of cardiac arrest or respiratory failure. Other medical treatments can still be provided.
- A DNR is only for terminally ill patients. While many people associate DNR orders with terminal illness, they can be appropriate for anyone who wishes to avoid resuscitation, regardless of their overall health status.
- Once signed, a DNR cannot be changed. This is a misconception. A DNR order can be revoked or modified at any time by the patient or their designated representative.
- Emergency responders will ignore a DNR. Emergency personnel are trained to respect DNR orders. If a valid DNR form is present, they will not perform resuscitation efforts.
- A DNR is the same as a living will. While both documents relate to end-of-life care, a living will outlines a person's wishes regarding medical treatment, while a DNR specifically addresses resuscitation efforts.
- Only doctors can fill out a DNR. While a physician's signature is required, patients can initiate the process and discuss their wishes with their healthcare provider.
- A DNR order is only valid in Ohio. DNR orders can vary by state. While Ohio has its own specific DNR form, other states have different regulations and forms that must be followed.
- Having a DNR means giving up on life. Many people view a DNR as a way to maintain dignity and avoid unwanted suffering. It is a personal choice reflecting one's values and preferences regarding end-of-life care.
Being informed about these misconceptions can help individuals make better decisions regarding their healthcare preferences. Understanding the nuances of a DNR order is vital for ensuring that one's wishes are honored.
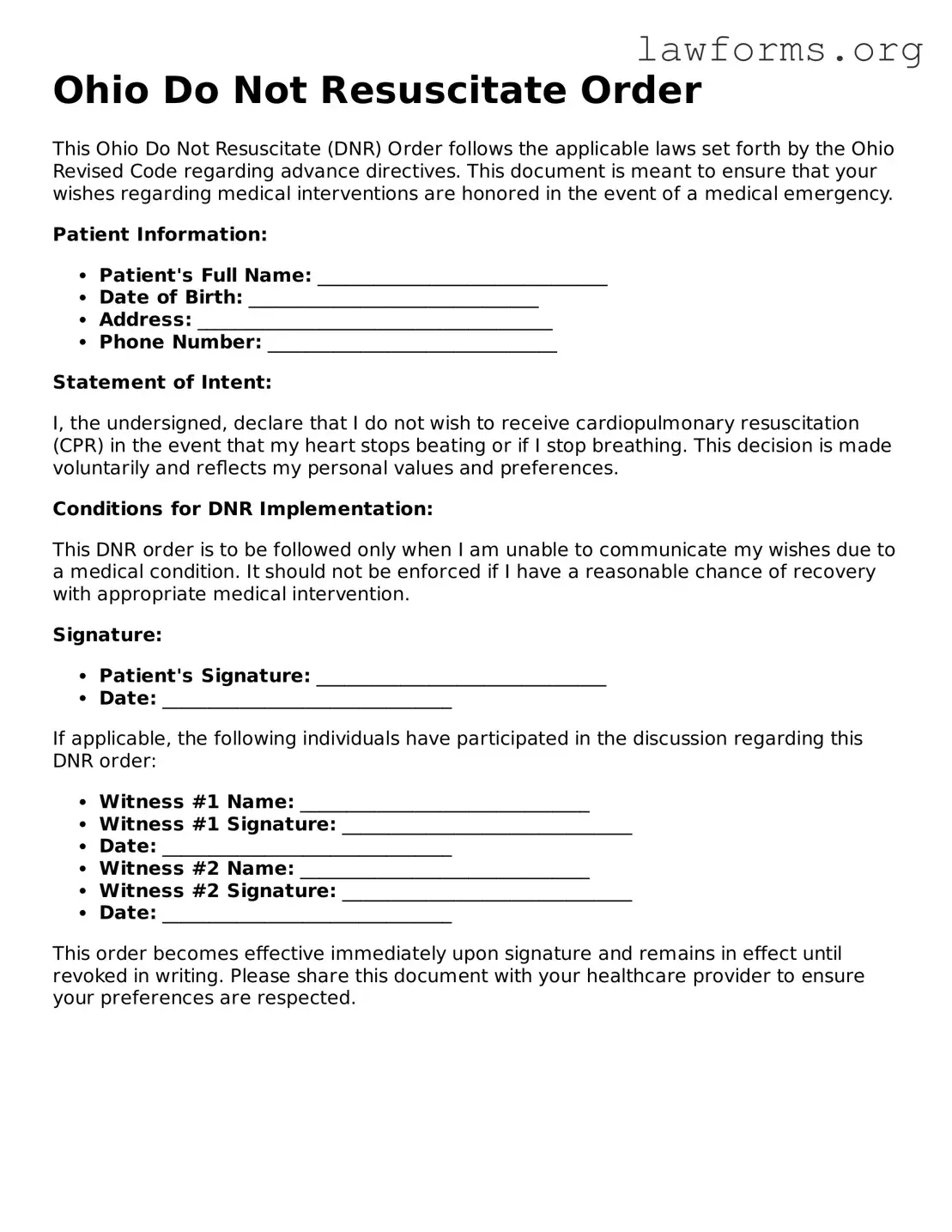
Preview - Ohio Do Not Resuscitate Order Form
Ohio Do Not Resuscitate Order
This Ohio Do Not Resuscitate (DNR) Order follows the applicable laws set forth by the Ohio Revised Code regarding advance directives. This document is meant to ensure that your wishes regarding medical interventions are honored in the event of a medical emergency.
Patient Information:
- Patient's Full Name: _______________________________
- Date of Birth: _______________________________
- Address: ______________________________________
- Phone Number: _______________________________
Statement of Intent:
I, the undersigned, declare that I do not wish to receive cardiopulmonary resuscitation (CPR) in the event that my heart stops beating or if I stop breathing. This decision is made voluntarily and reflects my personal values and preferences.
Conditions for DNR Implementation:
This DNR order is to be followed only when I am unable to communicate my wishes due to a medical condition. It should not be enforced if I have a reasonable chance of recovery with appropriate medical intervention.
Signature:
- Patient's Signature: _______________________________
- Date: _______________________________
If applicable, the following individuals have participated in the discussion regarding this DNR order:
- Witness #1 Name: _______________________________
- Witness #1 Signature: _______________________________
- Date: _______________________________
- Witness #2 Name: _______________________________
- Witness #2 Signature: _______________________________
- Date: _______________________________
This order becomes effective immediately upon signature and remains in effect until revoked in writing. Please share this document with your healthcare provider to ensure your preferences are respected.
Key takeaways
Here are some important points to consider when filling out and using the Ohio Do Not Resuscitate Order form:
- The form must be completed and signed by a licensed physician.
- It is essential to clearly indicate the patient's wishes regarding resuscitation efforts.
- The order should be printed and kept in a visible location, such as on the refrigerator or in a medical file.
- Family members should be informed about the existence of the DNR order.
- Healthcare providers must be made aware of the DNR order to ensure it is honored.
- The form should be reviewed periodically to ensure it still reflects the patient’s wishes.
- Patients can revoke the DNR order at any time, provided they communicate this decision clearly.
- It is advisable to carry a copy of the DNR order when traveling or when receiving care outside of a familiar setting.
- Consulting with a healthcare provider can help clarify any questions about the implications of a DNR order.
Similar forms
- Advance Directive: Similar to a Do Not Resuscitate Order (DNR), an advance directive allows individuals to outline their healthcare preferences in advance. It can include decisions about resuscitation and other life-sustaining treatments.
- Living Will: A living will is a specific type of advance directive that details what medical treatments a person does or does not want if they become unable to communicate. Like a DNR, it addresses end-of-life care.
- Durable Power of Attorney for Healthcare: This document designates someone to make healthcare decisions on behalf of another person. It complements a DNR by ensuring that a trusted individual can advocate for the patient's wishes.
- Physician Orders for Life-Sustaining Treatment (POLST): POLST forms are medical orders that specify a patient's preferences for treatment in emergency situations. They are more detailed than a DNR and are designed for those with serious health conditions.
- Do Not Intubate Order: This order specifies that a patient should not be intubated in the event of respiratory failure. It aligns with a DNR by focusing on the patient's wishes regarding invasive procedures.
- Residential Lease Agreement: The Ohio PDF Forms provide an easy way for landlords and tenants to create a legally binding lease that outlines their rights and responsibilities.
- Comfort Care Order: This document prioritizes comfort measures over aggressive treatment. It shares the intent of a DNR by emphasizing the quality of life rather than prolonging it through medical interventions.
- Healthcare Proxy: A healthcare proxy allows someone to make medical decisions for another person. It works alongside a DNR by ensuring that the appointed individual understands and respects the patient’s wishes.
- End-of-Life Care Plan: This plan outlines the patient's preferences for care during their final days. Like a DNR, it focuses on the patient's desires and can include various aspects of medical treatment.
- Patient Bill of Rights: While not a directive, this document informs patients of their rights regarding medical treatment, including the right to refuse treatment. It supports the philosophy behind a DNR by empowering patients to make informed choices.